Dr Robert Hess: Long Covid After Vaccination

Dr Robert Hess – 03/23/2022
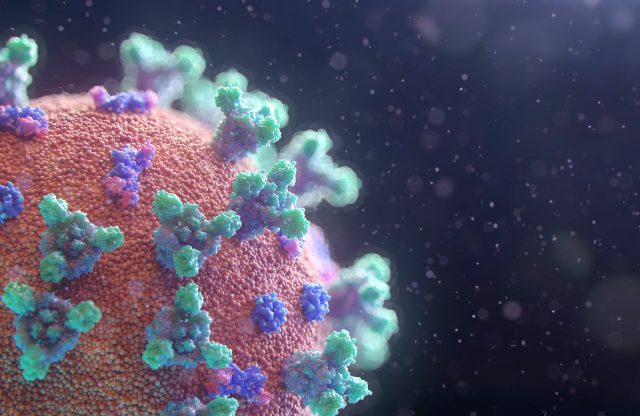
Dr Robert Hess: Long Covid After Vaccination
In rare cases, coronavirus vaccines may cause Long Covid–like symptoms.
As mentioned the symptomatology of this condition can be very similar to the side-effects and possible long-term consequences of vaccination. While preliminary data suggests that getting yourself vaccinated significantly reduces your risk of succumbing to Long Covid, there have also been cases where vaccination has caused Long Covid-like symptoms – and for a lengthy period of time.
We always take a balanced view, so that our clients are optimally informed and can weigh up the available information accordingly. There are no official figures, nor have there been any large-scale studies on this phenomenon as yet, but the symptoms, the link to vaccination and the accounts given by those affected are currently being investigated by the National Institute of Health (NIH) and other researchers around the world.
Previous studies have been too limited in scope and have not allowed 100% conclusions to be drawn about whether any of the vaccines have caused some rare form of long-term health problem and, if so, by what mechanism.
Long Covid-like symptoms such as fatigue, brain fog, insomnia, headaches, blood pressure fluctuations and various others are currently being investigated for a possible link to the administration of a COVID-19 vaccine. A number of scientists and research institutes are looking into this matter, among them neuroimmunologist Avindra Nath, clinical director of the Neurological Diseases Institute of the U.S. National Institutes of Health (NIH). In the specialist journal Science, he posited “temporal associations” between vaccination and Long Covid symptoms, but he would not be drawn on whether there was an “etiological association” (i.e. a causative link). Studies conducted by Nath on around 30 case reports have so far remained unpublished, but publication is expected soon.
Much remains unclear about Long Covid, especially the cause of its non-specific symptoms. It is broadly assumed that there is an underlying persistent immune dysregulation, in other words a defective immune response. Some candidates for further research are beta-interferons, immunoglobulins, mini blood clots and autoantibodies.
The Science article also explores the role of autoantibodies – their importance is recognized not only in acute CoV infection, but also in Long Covid. According to recent studies, autoantibodies can be detected up to six months after infection, and as Harald Prüss, a neurologist at the German Center for Neurodegenerative Diseases (DZNE) and at the Charité Hospital in Berlin, writes in an as yet unpublished paper, they are capable of damaging brain tissue.
Experiments on animals have suggested that antibodies targeting the SARS-CoV-2 spike protein – the same protein that many vaccines use to trigger a protective immune response – could cause collateral damage. While searching for antibody therapies for COVID-19 in 2020, Harald Prüss and his colleagues discovered that, of the 18 antibodies they identified with strong efficacy against SARS-CoV-2, four also attacked healthy tissue in mice – an indication that they could trigger autoimmune problems.
Initial clinical data point in a similar direction. Last year, researchers testing people infected with SARS-CoV-2 found unusually high levels of autoantibodies, which can attack the body’s own cells and tissues. In the May 2021 issue of Nature magazine, immunologists Aaron Ring and Akiko Iwasaki and their colleagues at the Yale School of Medicine reported finding autoantibodies in acute COVID-19 patients that were targeting the immune system and brain. They are now investigating how long the autoantibodies persist and the extent to which they can damage tissues. In January of this year, Cedars-Sinai Medical Center cardiologist Susan Cheng and protein chemist Justyna Fert-Bober reported in the Journal of Translational Medicine that autoantibodies can still be present up to six months after infection, although the researchers did not link their persistence to long-term symptoms.
To find out whether such autoantibodies harm humans, scientists at the German Center for Neurodegenerative Diseases (DZNE) are testing cerebrospinal fluid from Long Covid patients for antibodies that react to brain tissue obtained from mice: if there is indeed a reaction, these antibodies could also attack human neural tissue. Prüss and his team have published a paper in which they describe finding autoantibodies in at least one third of these patients, which are capable of attacking mouse neurons and other brain cells.
In August 2021, a group at Northwestern University reported in an advance publication that, in patients with neurological complications after COVID-19, a subset of T cells is persistently activated, similar to how it would be in persistent SARS-CoV-2 infection, suggesting an aberrant immune response or a lingering virus.
Scientists investigating possible side-effects are faced with a dilemma: their work risks stoking opposition to vaccines that currently seem to be “safe and effective” (this statement cannot be made with 100% certainty. After all, we have only been vaccinating for about 2 years and we are therefore rather cautious with these statements). “You have to be very careful about associating COVID-19 vaccines with complications,” Nath cautions. “People can draw the wrong conclusions. The implications are enormous.” Complex and persistent symptoms like those experienced by most sufferers are even more difficult to study, because patients often don’t have a clear diagnosis.
At the same time, understanding these problems could help those who currently suffer from them and, if a link is found, help in the development of the next generation of vaccines, perhaps identifying the ones that pose a high risk of serious adverse events. “We shouldn’t be averse to adverse events,” is how William Murphy, an immunologist at the University of California, sums it up. In November 2021, he suggested in The New England Journal of Medicine that an autoimmune mechanism triggered by the SARS-CoV-2 spike protein could explain not only the Long Covid symptoms but also some rare vaccine side-effects, and he called for more basic research to investigate possible links. He also maintains that it is more important to reassure the public that everything is being done in research to understand vaccines than to just say everything is safe, an assertion that we also endorse.
In the meantime, many affected people feel they have been let down by the health care system. The issue is sadly neglected, poorly defined and also politically sensitive, so family doctors and hospitals have not yet taken any initiatives. Many would like to see a network of specialist outpatient clinics for people with Long Covid and Long Covid-like symptoms, sharing their knowledge and experience.
Long Covid symptomatology after vaccination seems to be rare so far. Nevertheless, this is a topic that needs to remain in focus and be subjected to greater in-depth investigation. Overall, there are still too many unknowns and therefore there are currently no approved and effective therapies on the market. Nevertheless, we are able to take preventive action. We have already adapted our prophylactic measures in this regard, and we will also revise our supplements. We are one step ahead in this regard and we have put together effective options exclusively for our clients.
If you have any questions about Long Covid or specific symptoms, please do not hesitate to contact your consultant. We will continue to monitor this issue closely and to update our knowledge.