Dr Robert Hess: Best medication yet?

Dr Robert Hess – 01/20/2022
Dr Robert Hess: Best medication yet? Paxlovid a potential gamechanger
Paxlovid received emergency approval in the USA just before Christmas, and it got the all-clear for use in Europe as early as January. This new medication could help reduce the number of people who fall severely ill with COVID-19, but supply shortages and manufacturing problems are so far hindering widespread distribution.
Taken early enough after a diagnosis of COVID-19, paxlovid could dramatically reduce the risk of severe illness. Its manufacturer, Pfizer, claims that the likelihood of hospitalization or death for high-risk patients following an infection is reduced by almost 90 percent. Many in the medical profession are now hoping for its rapid and widespread deployment. Indeed, Germany and other European countries will probably begin using paxlovid before it is officially approved by the European Medicines Agency (EMA). However, it will not be clinicians who administer paxlovid to their patients. Ideally, the drug will avert the situation where infected patients have to go to hospital in the first place. It will therefore be prescribed primarily by family doctors. In our opinion, the great advantage of Paxlovid is its convenience and ease of use, i.e. as a tablet that infected individuals can take at home.
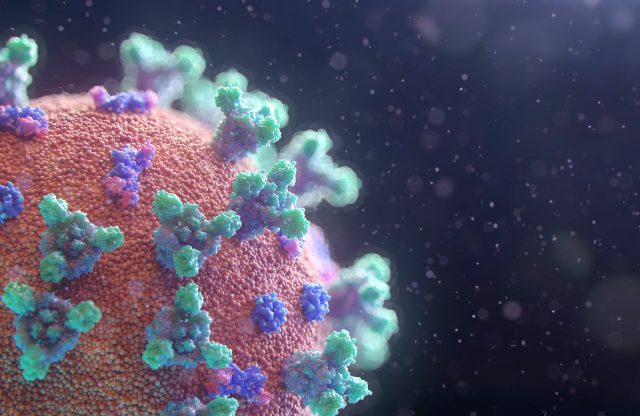
Paxlovid is an antiviral medication against COVID-19 consisting of two substances. The actual active ingredient, newly developed by Pfizer, is called nirmatrelvir. This inhibits 3CL protease, a molecule that Sars-CoV-2 needs to replicate in body cells. This mechanism of action has a major advantage: the gene segment that codes for this protease is only changed at one site in Omicron compared with Delta. We therefore have reason to believe that paxlovid is also effective against the new variant. And according to Pfizer, its effectiveness has also been indicated by initial laboratory tests. The other active ingredient contained in paxlovid is ritonavir, a substance that is also used in the treatment of HIV. Ritonavir ensures that nirmatrelvir is broken down more slowly and can therefore act for longer. The two elements are dispensed as separate tablets in the package of paxlovid. Infected patients who are deemed eligible for the drug must take two doses of nirmatrelvir and one of ritonavir twice a day for five days.
Paxlovid has been dubbed a potential gamechanger the basis of interim study results published by Pfizer at the beginning of November 2021. In mid-December, the company then issued a further announcement confirming these initial good results. According to the report, the drug is highly efficient in averting the need for emergency treatment and/or in preventing death among COVID-19 patients with mild or moderate symptoms who have not yet been hospitalized. In high-risk patients, paxlovid reduced the relative risk of hospitalization or death by almost 90 percent.
While only five of 697 people in the paxlovid test group required emergency treatment within four weeks (equivalent to 0.7 percent), among those who received a placebo, 44 out of 682 (equivalent to 6.5 percent) had to be admitted to hospital. Nine test subjects from the placebo group died from COVID-19, while there were no coronavirus deaths in the paxlovid group. These results apply to subjects who took paxlovid within three days of symptom onset, according to the news release. However – and this is very good news – Pfizer reports that efficacy is just as good when the first tablet is taken within five days of symptom onset. This considerably extends the window of opportunity.
Unlike molnupiravir, another antiviral drug we reported on a few weeks ago, estimates of paxlovid’s efficacy have not been downgraded. Merck & Co, the company that manufactures molnupiravir, had initially claimed that its product reduced the relative risk of severe COVID-19 by approximately 50 percent, but a subsequent review of the study results showed only a 30 percent reduction.
Based on everything we know so far, paxlovid looks the best of the available options. However, we must remember that there are still no published trial data. Pfizer has submitted its results to a medical journal for publication, but they are not yet open to public scrutiny. In order to better assess paxlovid, we require far more data, for example identifying the type of patients who most strongly benefit from treatment with the drug. The over-65s, who are automatically at greater risk due to their age, accounted for only 11.4 percent of the test subjects in an interim evaluation, and people over 75 made up only 2.9 percent of the sample. Furthermore, only unvaccinated individuals participated in the study. Since most of my clients are vaccinated, it is also important to see how effective paxlovid is among this population.
In terms of side-effects, paxlovid performed relatively well in the study. Apart from the more or less “usual” side-effects of drugs, such as diarrhea or vomiting, there were no unforeseen adverse reactions. The bigger problem with paxlovid is likely to be from another source, namely drug-drug interactions (DDIs).
The ritonavir component of paxlovid ensures that the actual active ingredient nirmatrelvir is broken down more slowly and can therefore take effect over a longer period. This happens because ritonavir inhibits an enzyme complex in the liver that is used to metabolize and break down many drugs in the body. And this, in turn, can cause these drugs to remain in the body in excessive concentrations. Other mechanisms associated with paxlovid consumption can also cause certain drugs to be broken down more quickly than normal, so that they work either inadequately or not at all. These interactions affect a wide variety of medications, but especially those prescribed for cardiac arrhythmias, antidepressants, cholesterol-lowering drugs, anticoagulants and certain antibiotics. We would therefore ask our clients to inform us in advance in the event of infection and a proposed course of paxlovid. We will then check and reconcile possible interactions with other medications.
And what about vaccination status?
The Pfizer study initially included only high-risk unvaccinated volunteers. Another study is currently analyzing the effectiveness of paxlovid in low-risk unvaccinated individuals and in vaccinated people with breakthrough infections. Nevertheless, vaccinated people will also be eligible to receive the medication.
The bigger problem in this context is availability and the inevitable triage scenarios, especially in the United States where doctors are already complaining about supply bottlenecks.
The U.S. government procures paxlovid centrally and allocates supplies to federal states where local health officials decide on distribution and on the guidelines to be issued to doctors. However, supplies have already been exhausted. The city of New York, for example, received about 1,300 paxlovid treatments at the end of December, but according to a spokesperson for Alto Pharmacy, which distributes the city’s supplies, these were used up within a week. We are reliably informed that New York City currently has no paxlovid in stock. Last Tuesday, the U.S. government doubled its paxlovid order, though we don’t expect supplies to last until April.
So while it is relatively easy to get a vaccine, there is likely nowhere near enough paxlovid to treat every at-risk individual who becomes infected. Manufacturing the drug also takes time, because producing the nirmatrelvir component is a complex multi-step process that takes months. Pfizer plans to produce up to 120 million units of paxlovid by the end of 2022. This sounds like a lot at first, but given the global demand, it is a drop in the ocean.
And it is not only paxlovid that is suffering from supply shortages. There are also problems with the procurement of proven monoclonal antibody therapy. Throughout most of the pandemic, monoclonal antibodies – a treatment generally administered intravenously in hospitals or clinics – have been the primary intervention for recently infected patients. The two most common types of monoclonal antibodies (casirivimab/imdevimab and etesevimab/bamlanivimab) do not work well enough against the Omicron variant. There is a third antibody treatment, sotrovimab, manufactured by GSK and Vir Biotechnology, that is effective against Omicron. However, the U.S. government had ordered only about 450,000 treatment units to date, many of which have now been used or have not yet been distributed to the state governments. On 12th January, the U.S. government announced in a press release that it had ordered an additional 600,000 units of sotrovimab.
Paxlovid can only become a gamechanger and GSK’s MAB therapy can continue in a supportive role if these treatments are made as widely and easily accessible as possible. Currently, the system only favors those who have the time, energy and knowledge to seek out treatments.
We will continue to share our assessment of the situation with you. If you find yourself in the situation of needing paxlovid or MAK therapy, please contact us beforehand so that we can talk through all the options and tailor them to your individual circumstances.